The space around the thing: why products alone won’t transform healthcare
To deliver transformation in healthcare, you must design for the space around the thing
The latest spending review reiterated the Government’s focus on improving health outcomes nationally. Key strategies to support this goal include a focus on prevention, reducing health inequalities and utilising digital to provide more efficient and effective services. These goals directly relate to the work we’ve been doing in digital screening with NHS England.
Since late 2024 and early 2025, we’ve been working in NHS England’s Transformation Directorate, specifically within the Digital Prevention Services Portfolio, supporting digital screening programmes. It’s been our first time working in healthcare – and what a learning curve it’s been.
We’ve been in Business Change roles, working alongside product teams who are delivering digital services that support screening. This has put us in a unique position. On one hand, we’re close to the digital products being developed. On the other, we’re focused on the much messier, often invisible part: how these products will actually land and be used in the real world.
This blog post series is about that second part – the part we’ve come to call “the space around the thing.”
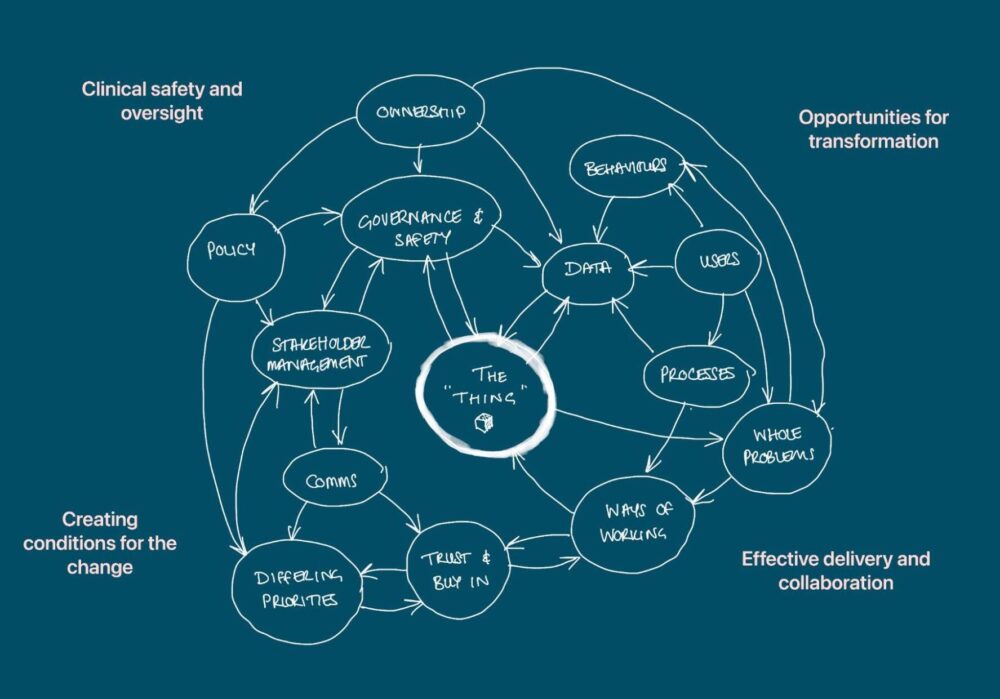
The thing vs. The space around the thing
In digital teams, especially in agile environments, there’s a strong focus on the thing – the product, the feature, the user need. And rightly so. But in our experience, you can build the best product in the world, and still have it go nowhere. Why? Because you didn’t design for the environment it’s entering. This is even more pertinent when delivering in the NHS.
The NHS environment is especially complex. It’s governed by opaque, interwoven factors – structures, behaviours, legacy systems, safety protocols, policies, culture, and people. And when those forces aren’t understood, or accounted for, even the best designed product will struggle to survive rollout.
And in healthcare, that ecosystem can be ambiguous, ever-shifting, and full of good reasons to resist change.
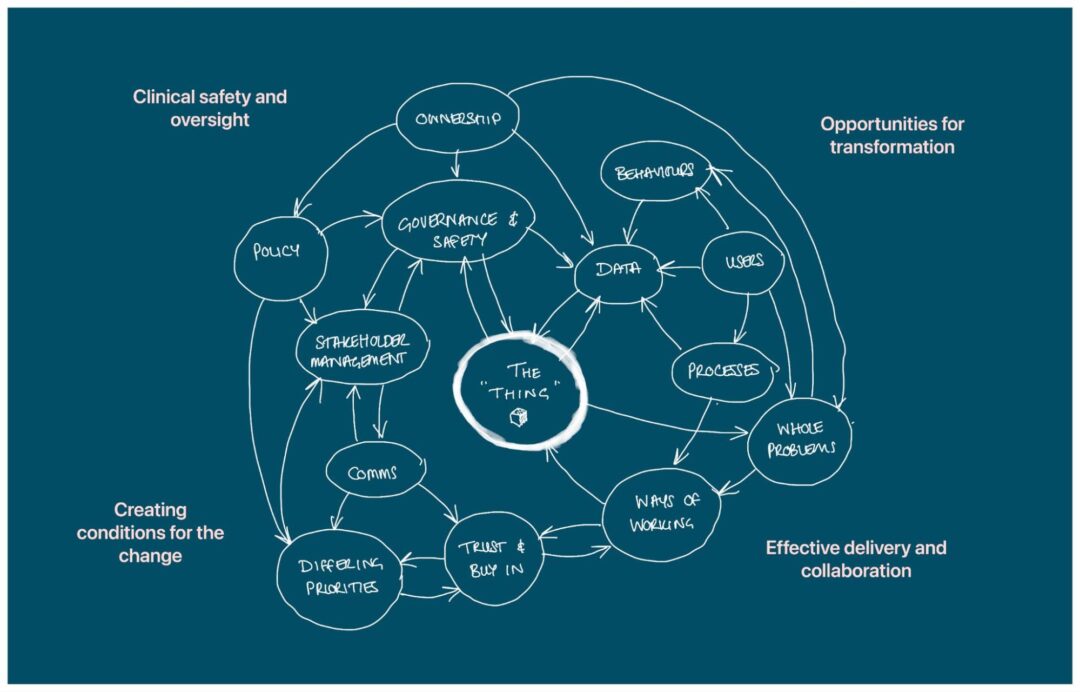
Image above illustrates the space around the thing
Creating space for transformation
Transformation in this space won’t succeed by digital alone. It demands a deep understanding of the whole system – how people work, how decisions get made, where accountability lies (or doesn’t), and how trust is built over time. Operating as Business Change Leads has required us to be adaptable to the needs of the programme, vigilant to opportunities to influence and comfortable working with ambiguity.
This might mean:
- understanding the ecosystem in which a product will be used, the barriers and opportunities for impact
- supporting good decisions through research, analysis and storytelling
- helping teams find clarity amongst shifting circumstances
- establishing good relationships across digital teams, and across the NHS
- identifying and engaging with decision makers
- creating tools that make it easier for teams to do what they need to do
- providing insight and reflections to senior leadership, helping to join the dots
- learning about and operating within existing non-digital processes (clinical safety, service specifications etc.)
- sharing approaches and ways of working
We’re starting to see national programmes take a more honest, long-term approach. Pathway leads, for example, are now openly talking about transformation over 4 years rather than 4 months. That shift in narrative is key. It creates space to talk about the invisible, slow, systemic work that must underpin any meaningful change.
What this series will cover
In this blog post series, we’ll share some of the invisible work we’ve been doing in digital screening – and what it’s taught us. Some of the topics we’ll explore:
- Clinical safety and governance: How traditional models can clash with agile practices, and how to bridge that divide.
- Legacy tech and risk aversion: Why switching off old systems is harder than it looks (and how we’ve approached it).
- The role of data: Why shared definitions and standards matter, particularly when operating at scale.
- Integrated care boards (ICBs): Their independence, their influence, and why stakeholder engagement is everything.
- Complexity on top of complexity: How misaligned language, ownership ambiguity, and differing delivery models all stack up.
- Whole problems, not isolated features: Why service design and systems thinking are critical in healthcare.
Through all of this, we’ll keep returning to that central idea: that to deliver transformation in healthcare, you must design for the space around the thing.
It doesn’t always have a name, this work. But it’s essential.